Post Test Kardio
- Post Test iPass berisi soal pilihan ganda dengan waktu ujian 60 menit.
- Peserta diharapkan mengerjakan try out dengan sungguh – sungguh sebagai simulasi ujian PPDS.
- Try out hanya dapat dilakukan 1 kali untuk satu akun peserta.
- Nilai post test dan jawaban benar akan ditampilkan di akhir sesi post test
- Semua soal wajib dijawab untuk dapat mengakhiri post test
Tryout Summary
0 of 50 Questions completed
Questions:
Information
You have already completed the tryout before. Hence you can not start it again.
Tryout is loading…
You must sign in or sign up to start the tryout.
You must first complete the following:
Results
Results
0 of 50 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 50
1. Question
Mid diastolic rumble in the tricuspid region is found in which of the following?
CorrectIncorrect -
Question 2 of 50
2. Question
A 25-year-old woman has a 2/6 ejection systolic murmur best heard in the second left intercostal space with normal S1. The S2 is split during inspiration, and P2 intensity is normal. No apical or parasternal heave. The murmur diminishes during expiration and standing up. What is the murmur likely due to?
CorrectIncorrect -
Question 3 of 50
3. Question
Which one of the following antihypertensive medications might you use to try and prevent new-onset atrial fibrillation?
CorrectIncorrect -
Question 4 of 50
4. Question
Which is not a cause of chronic cor pulmonale?
CorrectIncorrect -
Question 5 of 50
5. Question
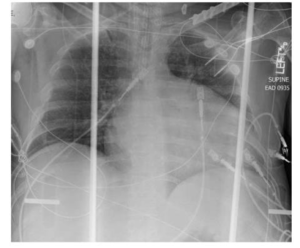
A 39-year-old male presented to the hospital after a cardiac arrest at home. He was brought to the hospital and had a chest X-ray. What does the chest X- ray show?
CorrectIncorrect -
Question 6 of 50
6. Question
Most common cause of kussmauls sign is?
CorrectIncorrect -
Question 7 of 50
7. Question
A 37-year-old man presents with pneumonia and a temperature of 39°C. He has no chest pain but a routine ECG is performed and is shown below.
 CorrectIncorrect
CorrectIncorrect -
Question 8 of 50
8. Question
Central venous pressure and wave forms are best appreciated in?
CorrectIncorrect -
Question 9 of 50
9. Question
36-year-old woman presented with an 8-month history of progressive exer- tional dyspnea. Physical examination revealed heart rate of 74 bpm, regular, BP 126/78 mmHg, no pedal edema. JVP and carotid upstroke were normal. Cardiac auscultation revealed normal S1, an accentuated P2 with narrow splitting of S2, an ejection click, and a 2/6 ejection systolic murmur. What is the likely diagnosis?
CorrectIncorrect -
Question 10 of 50
10. Question
Potassium sparing diuretics acts at?
CorrectIncorrect -
Question 11 of 50
11. Question
You review a 55-year-old woman in clinic who has been referred by her GP with recent chest pains. You feel that the nature of the pains is atypical for ischaemia although they are reproduced with exertion. She has no identifiable risk factors for ischaemic heart disease and the resting ECG is normal. What would you recommend?
CorrectIncorrect -
Question 12 of 50
12. Question
Continuous vascular murmur is heard when?
CorrectIncorrect -
Question 13 of 50
13. Question
What is the increase in myocardial contractile force with acute increase in afterload called?
CorrectIncorrect -
Question 14 of 50
14. Question
Best investigation for pericardial disease is?
CorrectIncorrect -
Question 15 of 50
15. Question
Which of the following statements is true regarding non-ST elevation acute coronary syndromes (nSTE-ACS) compared with ST elevation myocardial infarctions (STEMi)?
CorrectIncorrect -
Question 16 of 50
16. Question
Valvular function is best assessed by?
CorrectIncorrect -
Question 17 of 50
17. Question
You have been referred a 65-year-old man whom the GP has been struggling to manage. For the last year his clinic blood pressure recordings have been persistently around 50/90 mmHg, but he claims to suffer from the ‘white coat’ phenomenon, with home recordings of around 135/90 mmHg which you are satisfied have been undertaken appropriately. He is otherwise healthy, having implemented dietary changes and increased his exercise over the last year, but smokes and intends to continue. What do you recommend?
CorrectIncorrect -
Question 18 of 50
18. Question
One of your patients has small vessel coronary disease which is not suitable for revascularization. They are still experiencing class 2 angina particularly in the evening despite bisoprolol 10 mg od. Blood pressure is 135/90 mmHg. What would you recommend next?
CorrectIncorrect -
Question 19 of 50
19. Question
Most common cause of heart failure is?
CorrectIncorrect -
Question 20 of 50
20. Question
A 29-year-old pregnant woman was found to a have a systolic murmur best heard in the second left intercostal space. It is rough and there was a palpable thrill in the same area and in the suprasternal notch. Patient is asymptomatic and has normal exercise tolerance. What is the likely explanation of the murmur?
CorrectIncorrect -
Question 21 of 50
21. Question
The side effects of the broad spectrum of calcium-channel blockers (CCBs) include the following, except:
CorrectIncorrect -
Question 22 of 50
22. Question
A 52-year-old African American male was admitted with complaints of shortness of breath and edema. He has a history of methamphetamine use. A chest X-ray was performed in the emergency room (ER). What does the chest X-ray show?
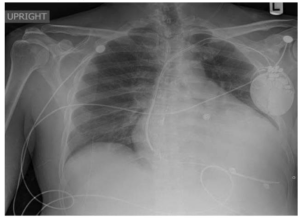 CorrectIncorrect
CorrectIncorrect -
Question 23 of 50
23. Question
A 62-year-old woman attends clinic following an ED attendance 6 weeks previously with a one-week history of palpitations. She was diagnosed with AF at the time and commenced on aspirin and a beta-blocker. Her echocardiogram showed no significant abnormalities and her ECG in clinic today confirms atrial fibrillation with a ventricular rate of 70 bpm. She continues to get occasional palpitations and would like to be considered for cardioversion. What do you advise?
CorrectIncorrect -
Question 24 of 50
24. Question
Abdominal aortic aneurysm is likely to rupture is its size is?
CorrectIncorrect -
Question 25 of 50
25. Question
Atherosclerotic plaque rupture is the most common event leading to clinically relevant ischaemia. Which one of the following statements regarding this process is not true?
CorrectIncorrect -
Question 26 of 50
26. Question
The GRACE risk model predicts in hospital mortality in ACS patients and includes Killip class, systolic blood pressure (BP), heart rate, age, and serum creatinine level. Which one of the following may be negatively correlated with mortality?
CorrectIncorrect -
Question 27 of 50
27. Question
On your ward round you review a patient who is 48 hours post anterior STEMi treated successfully with primary angioplasty. He has type 2 diabetes and hypertension. He is gradually improving, having initially suffered with heart failure. He still feels ‘chesty’ and auscultation reveals minimal basal crepitations. Echocardiography has revealed an ejection fraction of 40%. Blood pressure is 110/70 mmHg with heart rate 55 bpm at rest. Ramipril has been titrated to 2.5 mg bd with bisoprolol 2.5mg od. U&Es have remained normal. How would you improve his medical treatment?
CorrectIncorrect -
Question 28 of 50
28. Question
Which one of the following is a predictor of poor outcome in patients with infective endocarditis?
CorrectIncorrect -
Question 29 of 50
29. Question
57-year-old woman with known heart failure and EF 42% is reviewed in clinic. She is breathless on walking up one flightof stairs or half a mile on the flat. on examination, her BP is 130/90 mmHg and her heart rate is 75 bpm (SR, ECG QRS < 120 ms). Her chest is clear to auscultation. there are no signs of fluid overload. Her current medication is carvedilol 25 mgbd, furosemide 40 mg od, and digoxin 62.5 micrograms od. Her recent renal function tests are Na 141 mmol/L, K 5.1 mmol/L, urea 13.5 mmol/L, and creatinine 236 μmol/L. She has not previously tolerated an ACE inhibitor or spironolactone because of deteriorating renal function and hyperkalaemia. What would you do next?
CorrectIncorrect -
Question 30 of 50
30. Question
With regard to the pathogenesis of aortic aneurysm, which one of the following is the most important factor?
CorrectIncorrect -
Question 31 of 50
31. Question
Which one of the following statements regarding the new generation of antiplatelet drugs is not true?
CorrectIncorrect -
Question 32 of 50
32. Question
A 63-year-old male is admitted to the ED of a district general hospital with a short history of sudden-onset sharp back painand collapse. On examination he appears unwell, flushed, and diaphoretic. His blood pressure is 85/68 mmHg, his heart rate is 126 bpm, and his JVP is elevated. The emergency doctors suspect an acute dissection of the thoracic aorta which is duly confirmed on CT and extends from the sinuses of Valsalva to the aortic arch. A moderate pericardial effusion is noted and you are called to ‘drain this as the patient has cardiac tamponade’. What should you do?
CorrectIncorrect -
Question 33 of 50
33. Question
A 55-year-old female inpatient has recently been diagnosed with a transient ischaemic attack (TiA), which was confirmed by cerebral MRI. Echocardiography and carotid ultrasound are essentially normal. Her blood pressure during admission is 130/80 mmHg. What management do you suggest?
CorrectIncorrect -
Question 34 of 50
34. Question
Routine initial investigations in a 58-year-old patient with recently diagnosed Grade 3 hypertension should include all of the following, except:
CorrectIncorrect -
Question 35 of 50
35. Question
Patients with acute MI, may get which of the following types of AV conduction problems?
CorrectIncorrect -
Question 36 of 50
36. Question
A 65-year-old hypertensive non-diabetic has an eGFR <40. screening tests showed microalbuminuria and a normal renal ultrasound. Which class of antihypertensive medication should you instigate?
CorrectIncorrect -
Question 37 of 50
37. Question
A 67-year-old man with hypertension and diabetes presented with central chest pain lasting 30 min. There were no ECG changes, and cardiac markers were negative. The results of a stress perfusion study are shown in Figure 4.23. What will you recommend?
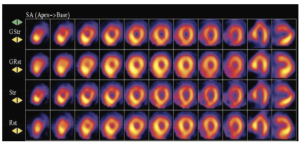 CorrectIncorrect
CorrectIncorrect -
Question 38 of 50
38. Question
What is the stress perfusion image shown in Figure 4.24 suggestive of?
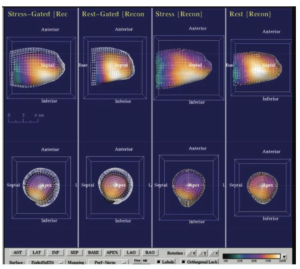 CorrectIncorrect
CorrectIncorrect -
Question 39 of 50
39. Question
Which one below is not associated with AV block?
CorrectIncorrect -
Question 40 of 50
40. Question
Most common underlying heart disease of sudden cardiac death is?
CorrectIncorrect -
Question 41 of 50
41. Question
A 65-year-old diabetic man with a previous history of myocardial infarction 3 years ago (no intervention required) is found to have atrial fibrillation. His LVEF is 55% and he has no cardiovascular symptoms. What would you advise him with regard to the best thromboprophylaxis?
CorrectIncorrect -
Question 42 of 50
42. Question
A 51-year-old farmer presents with low-grade fever and a recent history of weight loss. He has been investigated by his GP and general physicians but no cause has been identified for his symptoms. His inflammatory markers are raised and a TTE shows a 0.5 × 0.3 cm echogenic mass attached to the non-coronary cusp of the aortic valve. endocarditis is suspected, although multiple blood cultures are negative. Which one of the following organisms is the most likely cause of persistently negative cultures?
CorrectIncorrect -
Question 43 of 50
43. Question
Most common type of congenital heart disease in adults is?
CorrectIncorrect -
Question 44 of 50
44. Question
Guideline recommendation for ECG for patients presenting with chestpain to the ER is performance of ECG within how much time of arrival?
CorrectIncorrect -
Question 45 of 50
45. Question
For patients with ACS, what is the recommended duration of double antiplatelet therapy (DAPT)?
CorrectIncorrect -
Question 46 of 50
46. Question
In acute STEMI, primary PCI is preferred over fibrinolysis in which of the following situations?
CorrectIncorrect -
Question 47 of 50
47. Question
A 69-year-old male has a history of hypertension, diabetes mellitus controlled on long-acting insulin therapy, hypercholesterolemia, and past history of smoking. He is on optimal medical therapy. He has new onset of exercise-induced angina of 1 month duration. His primary care physician ordered a stress test. His stress test was interpreted as negative. He is now referred to you for further evaluation. What is the best test to order?
CorrectIncorrect -
Question 48 of 50
48. Question
Compared with atrial myocyte, ventricular myocyte is which of the following?
CorrectIncorrect -
Question 49 of 50
49. Question
What is the increase in myocardial contractile force with increase in preload called?
CorrectIncorrect -
Question 50 of 50
50. Question
Which of the following patients are reasonable candidates to evaluate for heart transplant?
CorrectIncorrect
